Disclaimer: While I am a Registered Dietitian and a Certified Diabetes Educator, this article is based on my personal experience with diabetes and birth control. It’s essential to work closely with your healthcare team to determine what is best for YOU!
As a Registered Dietitian and Certified Diabetes Educator, I have lived with type 1 diabetes since 1995. Through my personal journey of managing diabetes alongside family planning, I have witnessed firsthand how hormonal birth control can significantly affect blood sugar control, especially for those with type 1 diabetes. This article aims to shed light on the potential impacts of hormonal intrauterine devices (IUDs) on diabetes management and offer guidance to those navigating similar challenges.

A Personal Story
My journey with birth control has been marked by trials and errors. Each method presented its own set of challenges, but the experience with hormonal IUDs has been particularly noteworthy.
Progesterone Pills: A Rollercoaster Ride
My first encounter with birth control was with progesterone pills, which turned out to be a COMPLETE disaster for my blood sugar levels, mood, and overall sanity. My blood sugar soared into the 300s for no apparent reason, and emotionally, I was all over the place. One memorable (and rather comical) incident involved me bursting into tears over a lonely piece of cake in a restaurant display case. After just a few days, I knew this method was not for me. My poor fiancé (at the time) had no idea what he was getting into as I sobbed over that solitary piece of cake.
Estrogen-Based Methods: A Better Fit
After having my first child, I switched to the NuvaRing, an estrogen-based method. Unlike progesterone, estrogen did not seem to negatively impact my insulin sensitivity. In fact, it might have even improved it. Research supports this, suggesting that estrogen can enhance insulin sensitivity and reduce the risk of diabetes-related complications. However, estrogen can reduce milk supply if you are nursing, which is an important consideration for new mothers. I personally did not notice much of a difference and felt the ring was a bit intrusive, but did not want to try an IUD since I knew I wanted another baby in the somewhat near future.
Copper IUD: A Non-Hormonal Option
Between my second and third pregnancies, I opted for a copper IUD, a non-hormonal method. While it did make my menstrual cycles more painful (think tiny ninjas practicing their kicks), it did not interfere with my blood sugar control or emotional well-being.
The Progesterone IUD: A Challenging Experience
After my third child, I chose the Kyleena IUD, which contains a lower dose of progesterone compared to the Mirena IUD. Within three months, I noticed significant changes: my total daily insulin (TDD) increased by 25-30%, from an average of 32 units to 40 units. My carb ratio changed from 1:12 grams to 1:8 grams. Despite strict dietary control and regular exercise, I gained 5 pounds, experienced breakouts, and felt like I was going through puberty all over again. These changes were driving me up the wall, so I put on my detective hat and dove into some serious research.
The Turning Point
After extensive research, I concluded that the progesterone in the Kyleena IUD was likely the culprit behind these adverse effects. Progesterone is known to cause insulin resistance, leading to higher blood sugar levels and increased insulin requirements. I decided to have the IUD removed. Remarkably, within 24 hours, my insulin needs decreased, and my blood sugar remained stable even after indulging in carb-heavy foods.
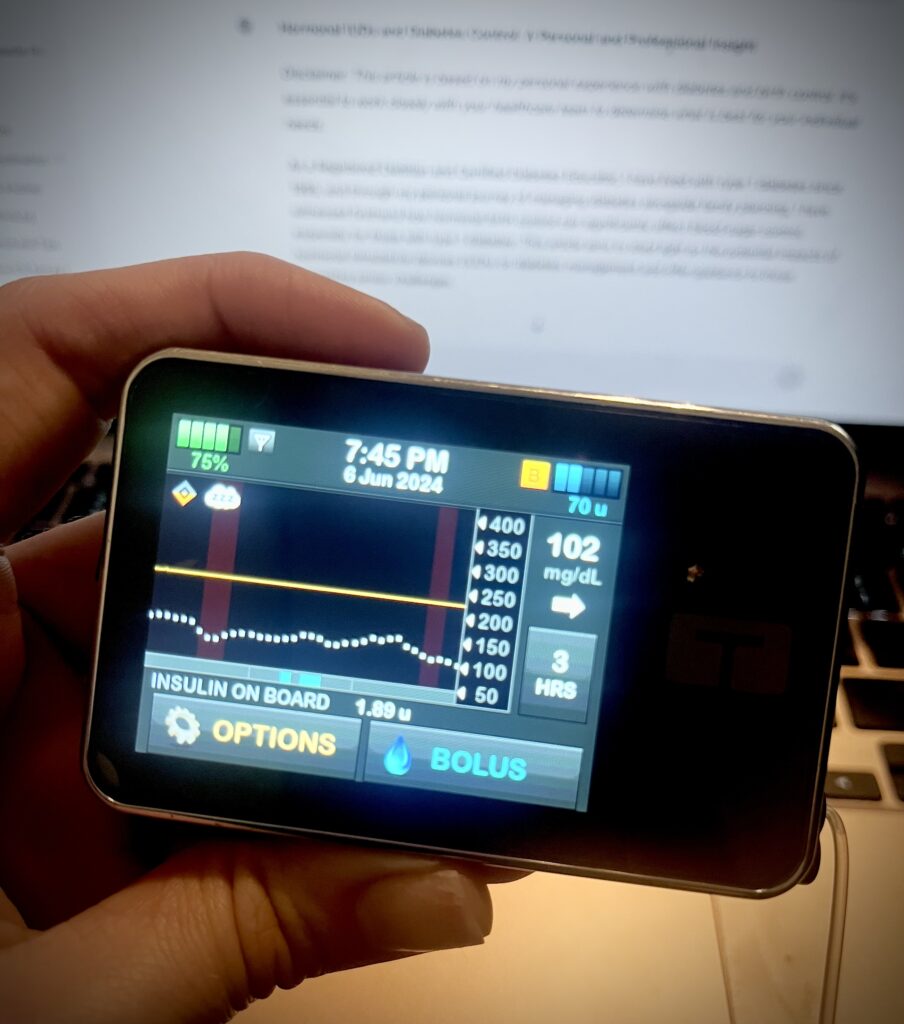
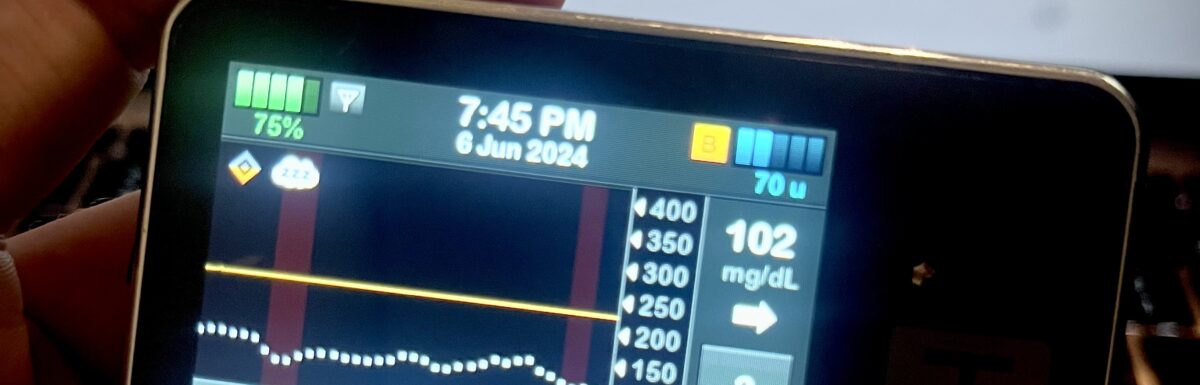
Picture of my Tslim X2 on the LOW Profile Setting after dinner (literally as I’m writing this article). This is the first day without the IUD, I indulged like there’s no tomorrow—I’m talking chili, CHIPS, ICE CREAM (yes, real ice cream, a rarity for me), and WATERMELON. And get this, I bolused less than half of what I needed for my previous dinner (just the day before), which was just keto egg waffles (without toppings) and a few wheat crackers. Yesterday my BG jumped to about 300 mg/dL.
Professional Observations
In my professional capacity, I have observed similar patterns in other women with diabetes who use hormonal IUDs. Increased weight gain and the need for more intensive insulin management are common complaints. Studies have shown that progesterone can exacerbate insulin resistance, which can be particularly challenging for women with diabetes. However, clinical research indicates that for many women, hormonal IUDs do not significantly impact insulin levels or HbA1c. This highlights the importance of individual responses and the need for personalized medical advice. Everyone should figure out the best fit for their own body and health needs.
Advice for Women with Diabetes
For women with diabetes, particularly type 1, it is crucial to weigh the pros and cons of hormonal versus non-hormonal birth control methods. Here are some recommendations:
- Monitor Your Blood Sugar Closely: Any change in medication, including birth control, can impact your blood sugar levels. Keep a close eye on your readings and adjust your insulin as needed.
- Consider Non-Hormonal Methods: Non-hormonal methods, such as copper IUDs or barrier methods, do not interfere with blood sugar control and may be a better option for some women.
- Work with Your Healthcare Team: Consult with your endocrinologist, diabetes educator, and gynecologist to find the most suitable birth control method for your individual needs.
- Prepare for Pregnancy: If you plan to become pregnant, aim to get your HbA1c down to 6.5% or below for at least six months before conceiving. This can improve the chances of a healthy pregnancy and reduce risks for both mother and baby.
Conclusion
The interplay between hormonal birth control and diabetes management is complex and highly individual. While some women may tolerate certain hormonal methods well, others may experience significant challenges. By sharing my personal and professional experiences, I hope to provide valuable insights for women with diabetes as they navigate their birth control options. Remember, informed decisions and close collaboration with your healthcare team are key to maintaining optimal diabetes control and overall well-being.

Schedule with Ariel Warren – Take Control of Your Diabetes and Your Life
Schedule a personalized consultation with Ariel Warren, Registered Dietitian and Certified Diabetes Educator, living with Type 1 Diabetes since 1995. Ariel specializes in insulin pumps, advanced diabetes management, nutrition, exercise, and weight loss.
We work through secure video calls, making it convenient to get expert guidance from home. Many insurance plans cover our visits. Usually just a copay or completely free!
Ariel will help you create a customized plan to stabilize your blood sugar, optimize insulin use, improve your metabolism, and reach your health and weight goals with diabetes.
Take control of your diabetes and live your best life. Book your appointment with Ariel today!