Living with insulin-dependent diabetes can be a challenge, to say the least! While medication and lifestyle adjustments are key to managing diabetes, emerging research suggests that certain foods, known for causing inflammation and food sensitivities, can contribute to insulin resistance. Which is just another factor that impacts our blood sugar control. This resistance affects how much the body responds to insulin, leading to changes in insulin requirements.
Understanding Insulin Resistance
Insulin resistance happens when your body’s cells become less responsive to the effects of insulin, making it harder for glucose to enter the cells. For people with insulin-dependent diabetes, this resistance can complicate blood sugar control and require higher doses of insulin. While insulin resistance is commonly associated with type 2 diabetes, it can also impact individuals with type 1 diabetes.
The Connection between Inflammation and Insulin Resistance
Inflammation is your body’s natural response to injury or infection. But when inflammation becomes chronic, it can disrupt various bodily functions, including insulin action. Some foods are known to promote inflammation, triggering an immune response and potentially leading to insulin resistance. We’re talking about foods high in processed sugars, refined grains, trans fats, and those with excessive omega-6 fatty acids (which are often found in vegetable oils). Which is why continually eating a highly processed diet can make stable blood sugar control next to impossible.
Not only that, but when insulin resistance occurs, the body needs to produce higher amounts of insulin to compensate for the reduced responsiveness. Insulin plays a crucial role in regulating the storage and usage of glucose as energy in the body. However, in the presence of insulin resistance, the excess insulin promotes the storage of glucose as fat in adipose tissue. Additionally, insulin resistance can lead to increased hunger and cravings, as the cells are not efficiently utilizing the glucose, resulting in higher levels of circulating sugar in the blood. This can contribute to overeating and the accumulation of excess calories, leading to weight gain over time. Moreover, insulin resistance can affect the metabolism of other hormones involved in weight regulation, such as leptin, which signals satiety. Altogether, these factors contribute to weight gain and the development of obesity in individuals with insulin resistance.
Which is very frustrating. Especially for those who work so hard to lose weight.
To determine your food sensitivities, an elimination diet is often recommended. This involves temporarily removing common allergens and potential trigger foods from your diet and then reintroducing them one at a time to observe any reactions. A benefit to diabetes (words not often said) is the ability to better track which foods cause inflammation and insulin resistance through the use of a Continuous Glucose Monitor (CGM). Keeping a detailed food diary in combination of your CGM reports, and working with a healthcare professional, such as a registered dietitian, can be very helpful and eye-opening when identifying patterns and narrowing down specific food triggers.
Food Sensitivities and Insulin Resistance
Have you ever had a food sensitivity or intolerance? It’s when your body struggles to digest or process specific foods. While food allergies cause an immediate immune response, food sensitivities can trigger a subtler immune reaction, leading to low-grade inflammation. Exposing your body to foods it’s sensitive to on an ongoing basis can potentially contribute to acute and chronic insulin resistance.
Common food sensitivities include gluten, dairy, eggs, soy, and certain nightshade vegetables like tomatoes, peppers, and eggplants. Remember, not everyone with insulin-dependent diabetes will have sensitivities to the same foods. Which only makes general diabetes nutrition education more confusing when people are trying to understsand their personal food sensitives that impact their insulin requirements.

Managing blood sugar levels is crucial for individuals with insulin-dependent diabetes to prevent short-term and long-term complications. However, if insulin resistance is present due to consuming inflammatory foods or having food sensitivities, controlling blood sugar can become more challenging.
Insulin resistance often requires higher doses of insulin to achieve adequate blood sugar control. Even when you’re sticking to your insulin regimen, you may experience frequent blood sugar spikes. This can increase the risk of hyperglycemia. On top of that, the necessary higher insulin doses used to counteract insulin resistance can potentially contribute to weight gain, making blood sugar management even trickier.
PERSONAL: My Food Sensitivities and How They Impact My Diabetes
With the use of my Dexcom, I am able to capture how certain foods impact my insulin requirements. For example, whenever I eat gluten, I have to gear myself for a wild ride with my blood sugar. And gluten used in a variety of foods impacts me differently. Which is super fun (sarcasm). Especially, when I’m the one controlling my insulin because of my deadbeat pancreas (aka Type 1 Diabetes).
I wanted to do an experiment to show how our blood sugar can be impacted when we eat our food sensitivities. Below is a picture of my Dexcom after eating some of my daughter’s vanilla graham cracker cookies. And yes, they were delicious.
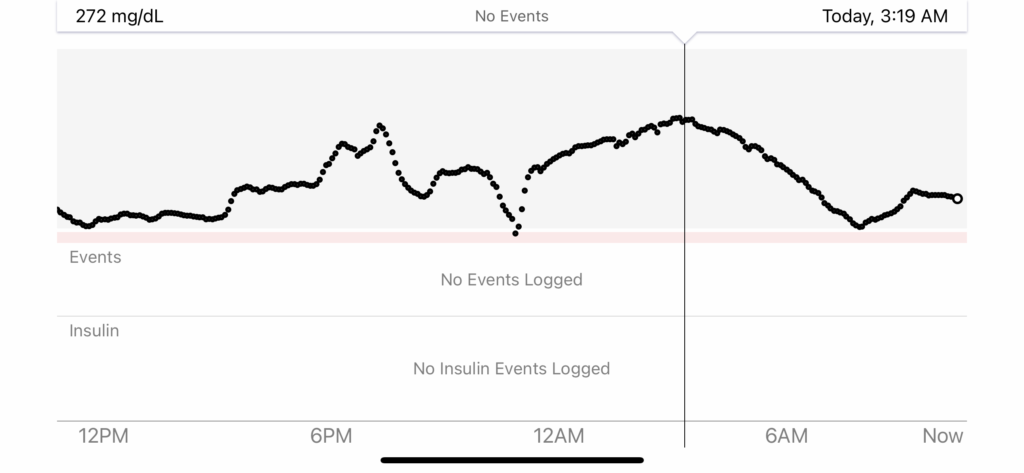
This was NOT a fun night. I ate the graham cracker cookies at 6:00 PM. I then went on a 3 mile walk with my family in order to combat the insulin resistance I knew would follow. The walk caused my BG to drop to 121 mg/dL. Soon after, it shortly began to rise. I knew it was going to be a minimum of 12 hours to get back to my usual insulin requirements and it was going to be a tough night.
During this event, I was using an Omnipod 5. With Omnipod 5, automated mode learns your insulin needs. Because I have extreme insulin resistance after consuming certain foods, I knew that my regular automated profile, would not be sufficient. Therefore, I had to switch out of automated mode, and use a “HIGH” profile in manual mode.
My usual total basal amount is about 12U per day, with the average basal at 0.5U per hour. When I am going through a bout of insulin resistance, I use a basal rate of 1.5 and as high as 3.0 u/hr. For this incident from the graham crackers, I used manual mode with a 3.0 u/hr basal.
Let that sink in. 3.0 u/hr is a whooping 150% increase in basal needs.
That was a tough night. But very interesting.
I rose to 272 mg/dL as my highest, and came back down to 146 mg/dL by 6:30 AM. The following morning, I got in a good workout to help expedite getting back to my normal insulin requirements.
TOTAL DAILY DOSE COMPARISONS
Below compares my normal total daily dose compared to the days when I eat sensitivity foods.
When I limit certain dairy and exclude gluten: 22.11U per day
When I do not limit/exclude any food: 43.2U per day
That’s nearly DOUBLE the insulin.
Discovering YOUR specific sensitivities can be done through keeping a food diary, trying an elimination diet, or seeking guidance from a Registered Dietitian.
Given the intricate relationship between food, inflammation, insulin resistance, and blood sugar control, it’s essential for everyone with insulin-dependent diabetes to take a personalized approach to their diet. Don’t hesitate to consult with a registered dietitian or healthcare professional experienced in diabetes management. They can help identify potential food sensitivities, create a tailored meal plan, and provide ongoing support and guidance.

Schedule with Ariel Warren – Take Control of Your Diabetes and Your Life
Schedule a personalized consultation with Ariel Warren, Registered Dietitian and Certified Diabetes Educator, living with Type 1 Diabetes since 1995. Ariel specializes in insulin pumps, advanced diabetes management, nutrition, exercise, and weight loss.
We work through secure video calls, making it convenient to get expert guidance from home. Many insurance plans cover our visits. Usually just a copay or completely free!
Ariel will help you create a customized plan to stabilize your blood sugar, optimize insulin use, improve your metabolism, and reach your health and weight goals with diabetes.
Take control of your diabetes and live your best life. Book your appointment with Ariel today!
References:
- American Diabetes Association. (2019). 6. Glycemic Targets: Standards of Medical Care in Diabetes—2019. Diabetes Care, 42(Supplement 1), S61-S70.
- Calder, P. C., Ahluwalia, N., Brouns, F., et al. (2011). Dietary factors and low-grade inflammation in relation to overweight and obesity. British Journal of Nutrition, 106(Supplement S3), S5-S78.
- Choudhury, M., & Friedman, J. E. (2009). Role of adipose tissue in insulin resistance and lipotoxicity. Adipocyte, 4(2), 121-125.
- Ehses, J. A., Perren, A., Eppler, E., et al. (2007). Increased number of islet-associated macrophages in type 2 diabetes. Diabetes, 56(9), 2356-2370.
- Esposito, K., Nappo, F., Giugliano, F., et al. (2003). Meal modulation of circulating interleukin 18 and adiponectin concentrations in healthy subjects and in patients with type 2 diabetes mellitus. American Journal of Clinical Nutrition, 78(6), 1135-1140.
- Feodoroff, M., Harjutsalo, V., Forsblom, C., et al. (2015). Finnish Diabetic Nephropathy (FinnDiane) Study Group. Food hypersensitivity in patients with type 1 diabetes and its relation to nephropathy. Diabetic Medicine, 32(12), 1634-1640.
- Fritsche, L., & Häring, H. U. (2008). Blood-based markers of glucose metabolism in diabetes mellitus. Experimental and Clinical Endocrinology & Diabetes, 116(9), 507-518.
- Hotamisligil, G. S. (2006). Inflammation and metabolic disorders. Nature, 444(7121), 860-867.
- Maedler, K., Spinas, G. A., & Donath, M. Y. (2002). Interleukin-1β induces islet apoptosis via multiple pathways. Journal of Endocrinology, 175(3), 307-312.
- Mari, A., Schmitz, O., Gastaldelli, A., et al. (2002). Meal and oral glucose tests for assessment of β-cell function: modeling analysis in normal subjects. American Journal of Physiology-Endocrinology and Metabolism, 283(6), E1159-E1166.
- Pedersen, B. K., & Febbraio, M. A. (2008). Muscle as an endocrine organ: focus on muscle-derived interleukin-6. Physiological Reviews, 88(4), 1379-1406.
- Roesch, L. F., Casella, G., Simell, O., et al. (2009). Influence of fecal sample storage on bacterial community diversity. Open Microbiology Journal, 3, 40-46.
- Sjöberg, K. A., & Roth, J. (2016). Nutrition and inflammation—impact on adipose tissue metabolism and insulin resistance. In Adipose Tissue Biology (pp. 195-216). Springer.
- Velloso, L. A., Eizirik, D. L., & Cnop, M. (2008). Nutrition and inflammation—impact on adipose tissue metabolism and insulin resistance. In Adipose Tissue Biology (pp. 195-216). Springer.

